This article was published in: Chinese Interventional Imaging and Therapeutics, Volume 20, Issue 1, 2023
Authors: Wang Zilin, Lian Jingge, Li Maolin, Ji Ying, Guo Xinyu, Li Kangan
To observe the multi-parameter evaluation of MRI to evaluate the effect of percutaneous microwave ablation (MWA) in the treatment of benign breast lesions.
■ Method
The breast MRI of 63 patients who received ultrasound-guided percutaneous MWA for breast benign lesions (a total of 66 lesions) before ablation and 6 months after ablation were retrospectively analyzed. Diameter, volume, T1 signal, T2 signal, diffusion weighted imaging (DWI) signal, apparent diffusion coefficient (ADC) and enhancement characteristics, and evaluate the therapeutic effect of percutaneous MWA according to the efficacy evaluation criteria for solid tumors.
■ Result
All 63 cases of 66 benign breast lesions were successfully ablated. Compared with before ablation, the longest diameter and volume of lesions decreased six months after ablation, T1 signal increased, T2 and DWI signal decreased, ADC increased, and enhanced signal decreased (all P<0.01). Six months after ablation, of the 66 lesions, 18 had complete remission, 46 had partial remission, and 2 had stable disease.
■ Conclusion
MRI multiparameters are helpful to evaluate the effect of percutaneous MWA in the treatment of benign breast lesions.
1. General Information
From January 2018 to December 2020, 63 patients with benign breast lesions who underwent ultrasound-guided percutaneous MWA in the First People's Hospital Affiliated to Shanghai Jiao Tong University School of Medicine were retrospectively included, all of them were female, aged 19-62 years, with an average ( 40.1±7.2) years old; a total of 66 lesions, of which 34 were breast fibroadenomas, 30 were breast lobular hyperplasia, and 2 were sclerosing mastopathy; including 36 left breast lesions (4 located in the upper outer quadrant of the left breast , 6, 6, 9 and 11 were located in the outer lower, inner upper, inner lower quadrants and the central area), 30 right breast lesions (4, 7, 5, 6 and 8 were located in the outer upper, outer lower , Inner Upper, Inner Lower Quadrants and Central Area).
Inclusion criteria:①Diagnosed as mammary imaging report and data by ultrasound examination, system grade 3 or 4A lesions, and then judged as 3 by contrast-enhanced ultrasound or breast MRI; ②MRI plain scan and diffusion weighted imaging were performed before and 6 months after MWA and enhanced scanning.
exclusion criteria:①Received breast-related surgery and other treatments before MR examination; ②MRI quality is not good; ③Severe underlying diseases and/or coagulation disorders exist.
2. Instruments and methods
1. Treatment method
The Siemens Sequoia C512 ultrasonic instrument was used as the guiding device. Firstly, conventional ultrasound scans the breast, observes the location, size and number of lesions, and determines the puncture point and puncture path.
Routine disinfection, draping, and local anesthesia with 5ml lidocaine, puncture the lesion under the guidance of ultrasound, and take appropriate amount of tissue for rapid pathological examination (for multiple lesions, take tissue separately for inspection) to determine its nature.
After confirming the diagnosis, under the guidance of ultrasound, inject 10ml ice saline and 5ml lidocaine mixture around the lesion, insert a 16G water-cooled circulating microwave ablation needle (Ego Medical) into the lesion, and connect a cold-circulating microwave tumor therapy instrument (Ego Medical) Medical treatment) perform MWA, choose fixed ablation according to the size of the lesion or perform multi-point ablation from inside to outside, from top to bottom, from deep to shallow, set the ablation power and time according to the specific situation, and perform multi-needle and multi-point ablation for larger lesions Multi-surface ablation, single multi-point ablation for multiple lesions;
Observe the echo situation at the position of the microwave needle tip during the period, and stop when the strong echo completely covers the lesion (that is, it has been fully ablated);
Immediately perform breast MR plain scan + enhancement, observe the T1WI, apparent diffusion coefficient (ADC) map and enhancement performance of the lesion, and judge whether the lesion is completely ablated, and the lesion no longer enhances or shows ring enhancement as complete ablation; if not completely For ablation, further multi-directional ablation is performed until complete ablation is achieved.
2. MR examination
Using PhilipsAchieva 3.0 TMR instrument and 7-channel breast dedicated phased array coil, breast MR scans were performed before ablation, immediately after ablation and 6 months. Ask the patient to lie prone on the test bed, so that the breasts on both sides hang naturally in the double holes of the coil;
Scan parameters: axial T1WI, TR609ms, TE8ms, slice thickness 5mm, FOV340mm×340mm, matrix 352×423, excitation times 1; axial fat suppression T1WI, TR400ms, TE8ms, slice thickness 5mm, FOV340mm×340mm, matrix 352×423 , excitation times 1; axial DWI, TR5098ms, TE70ms, b=0.1000s/mm², FOV340mm×340mm.
Dynamic contrast-enhanced MRI was performed after the plain scan was completed, the contrast agent GD-DTPA0.2mmol/kg body weight was injected through the cubital vein at a flow rate of 3ml/s, and 10ml of normal saline was injected at the same flow rate, and then continuous and uninterrupted enhanced scan was performed. TR4.2ms, TE2.1ms, FA10°, slice thickness 5mm, matrix 352×423, FOV 340mm×340mm, scan 7 cycles.
3. Image Analysis
Two physicians with 5 years of experience in breast MRI diagnosis with the title of deputy director or above respectively adopted a blind method to read the films. When there was a disagreement, another chief physician of the imaging department was asked to make an evaluation, and finally a consensus was reached through negotiation;
Measure the longest diameter of the lesion, and evaluate the lesion T1, T2, and DWI (refer to the method in the literature, for b=0s/mm2 DWI original image) by comparing the signal with the surrounding breast tissue for low, equal or high signal and its enhancement characteristics (none, mild or significantly enhanced), and placed the ROI with an area > 2mm² in the area where the signal of the largest layer of the lesion was relatively uniform on the ADC map automatically generated by the software, and the ADC was obtained, and the average value was obtained by repeating the measurement 3 times.
3DSlicer software was used to manually delineate the ROI of the lesion on DCE-MRI, and the volume of the lesion before and after 6 months of ablation was obtained.
4. Evaluate the curative effect of MWA
According to the MRI manifestations before and 6 months after ablation, the treatment effect was evaluated with reference to the efficacy evaluation criteria for solid tumors: complete remission, MRI showed that breast lesions completely disappeared or only showed flaky, cable-like signals, no enhancement in enhanced scans; partial remission, lesions The volume of the lesion is reduced by ≥50% compared with that before the operation, and the non-enhancement area of the lesion is ≥50% in the enhanced scan; the disease is stable, and the volume of the lesion is reduced by <50% or increased by <25% compared with that before ablation; the disease is progressing, and the volume of the lesion is increased by ≥25% compared with that before ablation %.
5. Statistical Analysis
SPSS26.0 statistical analysis software was used.
The measurement data conforming to the normal distribution are represented by -x±s, and those not conforming to the normal distribution are represented by the median (upper and lower quartiles). Paired samples t test or Wilcoxon rank sum test are used for comparison. Categorical data were compared using the Wilcoxon rank sum test.
Intra-observer correlation coefficient (measurement data) and unweighted Kappa test (categorical data) were used to analyze the consistency of evaluating the MRI performance of lesions between observers: 0.20<Kappa/ICC≤0.40 was considered moderate consistency, and 0.40<Kappa/ICC≤0.60 was considered Moderate consistency, 0.60<Kappa/ICC≤0.80 is strong consistency, 0.80<Kappa/ICC≤1 is strong consistency. P<0.05 means the difference is statistically significant.
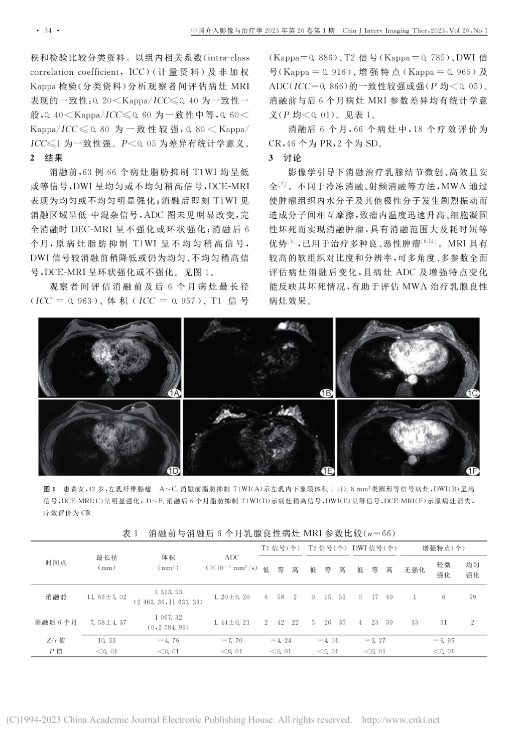
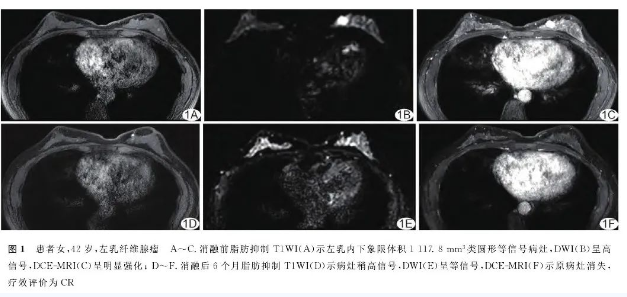
Before ablation, fat-suppressed 66 lesions in 63 cases showed low or isointensity on T1WI, DWI showed uniform or inhomogeneous slightly high signal, and DCE-MRI showed homogeneous or inhomogeneous enhancement; immediately after ablation, T1WI showed low-intensity in the ablation area Medium mixed signal, no obvious change in ADC map, DCE-MRI showed no enhancement or ring enhancement after complete ablation; 6 months after ablation, original lesion fat suppressed T1WI showed uneven and slightly high signal, and DWI signal was slightly lower than before ablation Or still homogeneous, heterogeneous slightly high signal, DCE-MRI showed ring enhancement or no enhancement. See Figure 1.
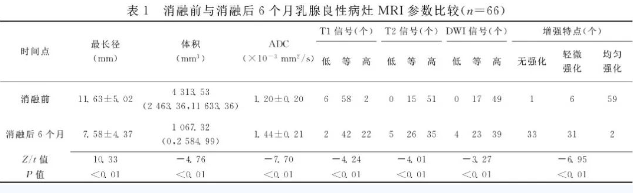
The longest diameter of the lesion (ICC=0.963), volume (ICC=0.957), T1 signal (Kappa=0.886), T2 signal (Kappa=0.785), and DWI signal (Kappa=0.916) were evaluated between observers before and after 6 months of ablation. ), enhanced features (Kappa=0.965) and ADC (ICC=0.866) had strong consistency (all P<0.05).
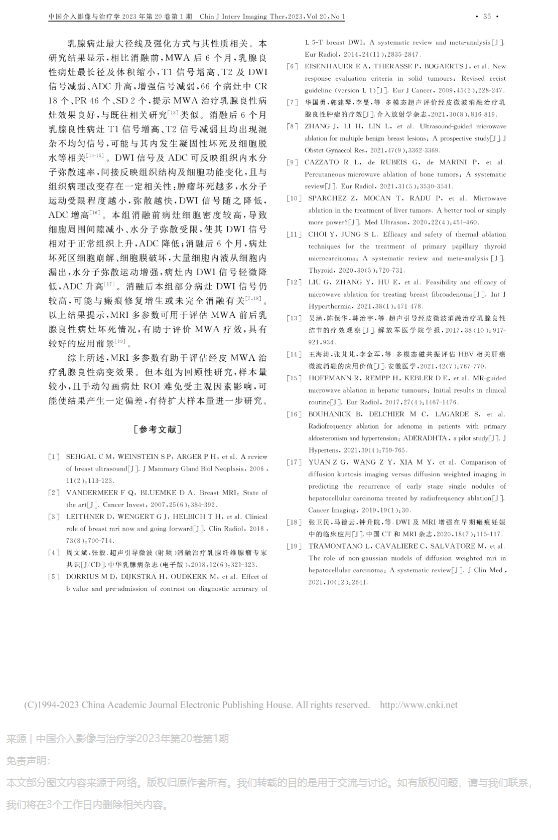
There were statistically significant differences in MRI parameters of lesions before and 6 months after ablation (all P<0.01). See Table 1. Six months after ablation, among the 66 lesions, 18 were CR, 46 were PR, and 2 were SD.
The imaging-guided ablation treatment of breast nodules is minimally invasive. Different from methods such as cryoablation and radiofrequency ablation, MWA causes water molecules and other polar molecules in the tumor tissue to vibrate violently to cause mutual friction between molecules, causing the temperature in the tumor to rapidly increase. The ablation of tumors is achieved by the elevation of the tumor and the coagulation necrosis of cells, which has the advantages of large ablation range and short time consumption, and has been used to treat a variety of benign and malignant tumors.
MRI has high soft tissue contrast and resolution, and can evaluate the changes of lesions after ablation from multiple angles and parameters, and the changes in ADC and enhancement characteristics of lesions can reflect their necrosis, which is helpful for evaluating the effect of MWA on benign breast lesions.
The maximum diameter and enhancement mode of breast lesions are related to their nature. The results of this study showed that compared with before ablation, six months after MWA, the longest diameter and volume of benign breast lesions decreased, T1 signal increased, T2 and DWI signal decreased, ADC increased, enhanced signal decreased, and CR18 out of 66 lesions , PR46, and SD2, suggesting that MWA is effective in treating benign breast lesions, which is similar to previous related studies.
Six months after ablation, the T1 signal of the benign breast lesions increased, the T2 signal decreased, and mixed and uneven signals appeared, which may be related to the occurrence of coagulation necrosis and cell dehydration. DWI signal and ADC can reflect the diffusion rate of water molecules in the tissue, indirectly reflect changes in tissue structure and cell function, and have a certain correlation with histopathological changes: the more tumor necrosis, the less restricted the movement of water molecules, and the faster the diffusion. The DWI signal decreases accordingly, and the ADC increases.
The density of the lesion cells in this group was high before ablation, resulting in the decrease of the space around the cells and the restriction of the diffusion of water molecules, so that the DWI signal increased and the ADC decreased compared with the normal tissue; Destruction, a large amount of intracellular fluid leaks from the cells, the diffusion movement of water molecules is enhanced, the DWI signal in the lesion is slightly reduced, and the ADC is increased.
After ablation, the DWI signal of some lesions in this group was still high, which may be related to scar repair hyperplasia or incomplete ablation.
The above results suggest that MRI multi-parameters can be used to evaluate the necrosis of benign breast lesions before and after MWA, which is helpful to evaluate the efficacy of MWA, and has a good application prospect.
In summary, MRI multi-parameters are helpful to evaluate the effect of percutaneous MWA in the treatment of benign breast lesions. However, this group is a retrospective study with a small sample size, and manually delineating the ROI of lesions is inevitably affected by subjective factors, which may cause certain deviations in the results, and further research is needed to expand the sample size.
The original text of the document ORIGINAL INFORMATION